NeoRoo, an integrated mobile app to improve care for premature babies in Kenya, was a finalist for the Innovation Prize at the 2021 Global Health and Innovation Conference. Sherri Bucher, PhD, presented on behalf of the NeoInnovate Collaborative Consortium. Although NeoRoo was not selected for the top prize, she said the process was instructive.
“It was great to be one of the six finalists for the Innovation Prize,” said Bucher, associate research professor of pediatrics at IU School of Medicine. “Developing the final pitch was an iterative, months’ long process. I learned a lot about how to design a 5-minute presentation for a social entrepreneurship audience.”
Bucher explained that NeoRoo is the latest digital health innovation co-developed by multidisciplinary partners from the United States and Kenya. It works in combination with NeoWarm and other mobile Helping Babies Survive powered by DHIS2 app development efforts. NeoWarm is a patented, wearable biomedical device for premature and low birthweight babies that includes a self-warming pouch and carrier, as well as a system to monitor vital signs and alert caregivers if the newborn’s body temperature fluctuates from a normal range.
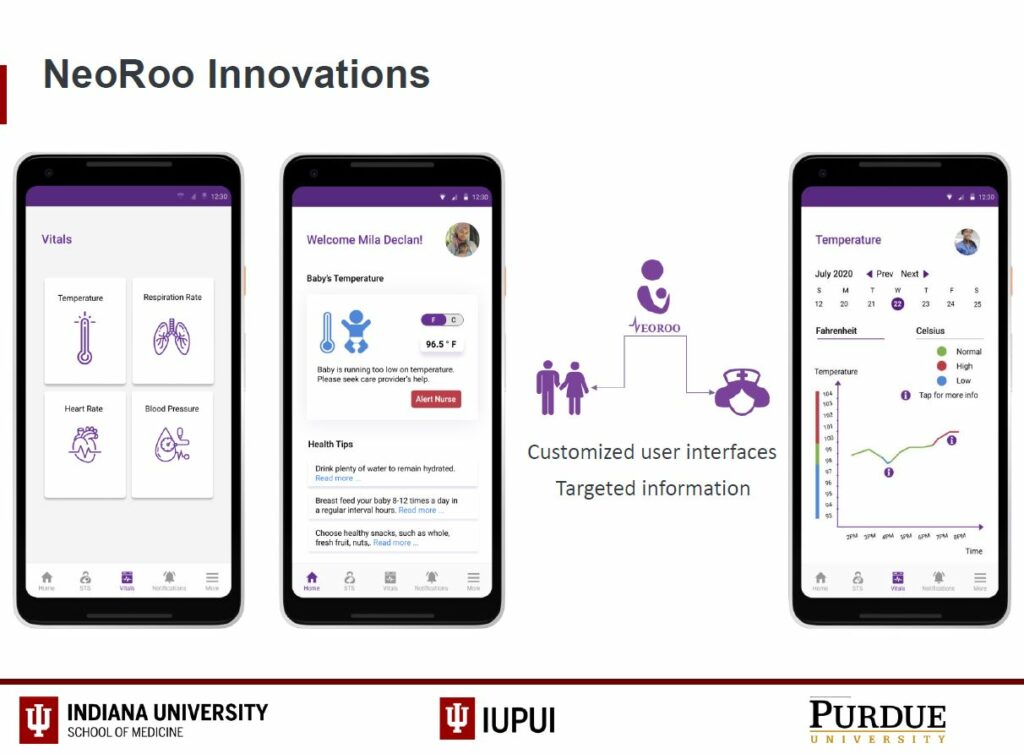
The NeoRoo app would provide customized user interfaces for both family caregivers and medical staff to monitor the temperature, respiration rate, heart rate and blood pressure of babies during kangaroo mother care (skin-to-skin contact). It would include automatic alerts if the baby’s vital signs are abnormal. For medical personnel, it would provide the ability to track multiple babies simultaneously as well the ability to set and track shared goals with caregivers. Over the next several months, with a grant from the division of neonatal-perinatal medicine, Bucher, students, and faculty collaborators will conduct participatory design interviews among healthcare providers based in Kenya and Indianapolis.
Geetha Priya Padmanaban designed the NeoRoo user interface. She is a Master’s of Science student in Human-Computer Interaction from the Purkayastha Lab for Health Innovation at the IUPUI School of Informatics and Computing.
The innovations aim to reduce newborn deaths by preventing hypothermia, a deadly complication for premature babies. Worldwide there are 15 million premature births and an estimated 2.1 million newborn deaths annually.
Last year, Bucher and her collaborators at Purdue University Weldon School of Biomedical Engineering and Moi University School of Medicine in Kenya received a $50,000 grant through the Global Health Reciprocal Innovation demonstration grant program from the Indiana Clinical and Translational Sciences Institute (CTSI) and IU Center for Global Health. The grant funded investigation of integrating KickSTART smartwatch technology originally developed to continuously monitor vital signs and detect overdose among adult opioid users into the NeoWarm device to monitor opioid-exposed babies in Indiana. Initial work has centered on adapting the KickSTART algorithms for use among neonates; soon, additional validation and verification testing will be conducted, using neonatal pigs as an animal model for premature babies.
Geetha Priya Padmanaban designed the NeoRoo user interface. She is a Master’s of Science student in Human-Computer Interaction from the Purkayastha Lab for Health Innovation at the IUPUI School of Informatics and Computing.
The continuous refinement and innovation process between investigators in Kenya and Indiana is an example of reciprocal innovation. In healthcare settings, reverse innovation refers to innovations and technologies designed and tested in under-resourced countries that are brought back to developed countries such as the United States to address important health challenges. These innovations are often cost-effective; easy to replicate, scale, and sustain; require minimal infrastructure; and can be tailored to local needs. However, reverse innovation is frequently seen as a one directional process with limited benefit to the under-resourced communities where the technology or innovation is developed.
Reciprocal innovation evolves this concept to create a two-way research agenda that provides mutual benefit to both sides and identifies high quality innovations from global health partnerships for demonstration, replication, and dissemination through a statewide system in Indiana and at partner sites globally.
“We are addressing a very well-defined, urgent problem that has global significance in many different settings,” said Bucher. “We didn’t build a solution and then go looking for a problem.”
The Indiana CTSI recently launched a reciprocal innovation online repository with information about past grant recipient and the innovations that have resulted. Each project includes information about the intervention, key facilitators, target population, process to implementation and how the innovation was scaled or transferred to other settings.
“We hope this repository will be a resource for ongoing innovation as well as an inspiration for future investigators to think about how their innovations can be expanded and adapted to address health challenges in other settings,” said Rish O’Brien, MPA, program manager for the global health reciprocal innovation initiative.
