 Assessing the up and downsides of Indiana’s Medicaid expansion plan known as HIP or “Healthy Indiana Plan” was the goal of a recently completed, community-engaged research study, led by Religious Studies Professor David Craig, Indiana University School of Liberal Arts at IUPUI, and a research affiliate with the Indiana Clinical and Translational Sciences Institute. The non-traditional, community-focused research team included leaders at First Baptist Church North Indianapolis, located on the city’s near northwest side and Shepherd Community Center on the east side, along with design researchers from the Herron School of Fine Art and Design and funding provided by Indiana’s Minority Health Coalition. Together they collected stories of neighbors’ and congregants’ experiences with HIP—just in time for Indiana’s proposed ten-year extension of the waiver that allows HIP to operate outside certain Medicaid rules.
Assessing the up and downsides of Indiana’s Medicaid expansion plan known as HIP or “Healthy Indiana Plan” was the goal of a recently completed, community-engaged research study, led by Religious Studies Professor David Craig, Indiana University School of Liberal Arts at IUPUI, and a research affiliate with the Indiana Clinical and Translational Sciences Institute. The non-traditional, community-focused research team included leaders at First Baptist Church North Indianapolis, located on the city’s near northwest side and Shepherd Community Center on the east side, along with design researchers from the Herron School of Fine Art and Design and funding provided by Indiana’s Minority Health Coalition. Together they collected stories of neighbors’ and congregants’ experiences with HIP—just in time for Indiana’s proposed ten-year extension of the waiver that allows HIP to operate outside certain Medicaid rules.
Listening to HIP members, what the research team found, is that many of the program’s success stories are marred by stories of individual challenges in navigating the program and attempting to advocate for better health and wellness by themselves.
Affordability is a key challenge. Indiana is the only state that requires people earning less than 50% of the Federal Poverty Level (about $700 per month) to pay premiums to receive full health benefits through HIP.
“At this income level, even payments of $1-2 per month are barriers for people’s enrolling in HIP Plus, the more comprehensive HIP plan,” said Craig.
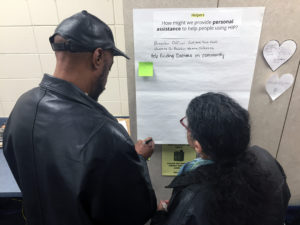
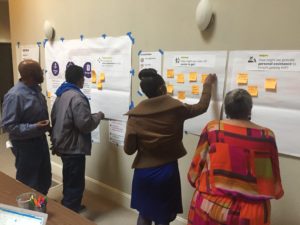
Study participants also reported more success obtaining and using HIP when supported by trusted advocates and community organizations.
“Sometimes you need to be heard. We need to know there’s somebody listening,” said a man, who was formerly homeless, in support of HIP.
He spoke these words in praise of three women, a nurse, a counselor, and a care coordinator, who listened to him and together they helped him through his recovery and into an apartment with furniture, pots, pans, and food.
“HIP creates add-ons. It brings more things to you. People think it’s just insurance; there’s more to HIP than you see,” he added.
Listening is a key component of the Monon Collaborative’s “Community Impact Hubs,” which are being formed through research projects like the one Professor Craig led evaluating HIP.
“We want to listen to understand the most pressing health issues in the community to help design and deliver solutions through our community impact hubs like the solutions proposed in the evaluation of HIP,” said Sarah Wiehe, MD, MPH and Director of the Monon Collaborative, a signature program of the Indiana Clinical and Translational Sciences Institute that connects community organizations, including universities, across the state in order to close health equity gaps.
The HIP research findings are conveyed in two easy to understand community-partner-produced videos and a final report.
This study illustrates the power of collaborative work between community and university. With the bottom line suggesting that HIP has the potential to positively impact many more lives if a relational and resource-supported approach to implementation is taken, versus one where members are left to navigate HIP alone and without many of the resources that others may take for granted.
