CDC 10-Step Pandemic Policy Response Plan, Recommends Enforcing Mask Mandates
On Friday, the Centers for Disease Control released a new, evidence-based “urgent battle plan” offering recommendations to local policymakers and public health agencies on how to respond to a COVID-19 pandemic that doctors and nurses state is overwhelming their facilities.
While vaccines are on the way, public health experts expect the weeks and months ahead to be particularly dangerous, as positive rates and hospitalizations continue to increase nationwide, cold weather forces more people indoors, and flu season goes into full swing. As the New York Times describes it, we are in the long darkness before dawn, and we will need to increase, not decrease, our reliance upon mask wearing, hand washing, social distancing and preventing crowds to get us through this time as safely as possible.
The agency seeks more uniform adoption of these best practices to maximize the effectiveness of response efforts. The authors state,
“No single strategy can control the pandemic; rather, a multipronged approach using all available evidence-based strategies at the individual and community levels can break transmission chains and address high levels of community transmission; reduce related illnesses, long-term sequelae, and deaths; and mitigate the pandemic’s economic impact.”
Included in the guidance are recommendations that states and local jurisdictions implement policies requiring (and enforcing) mask mandates in public spaces, and that people avoid indoor spaces outside the home (including indoor dining at restaurants).
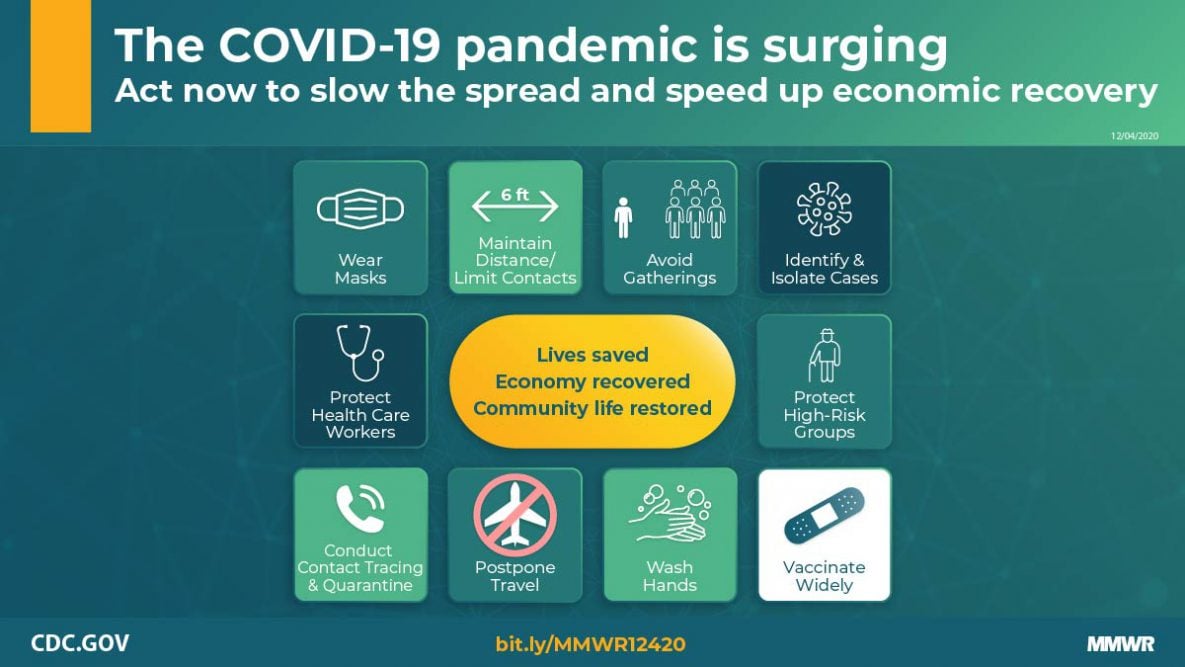
Below are a graphic and bullet points outlining the ten Recommended Public Health Strategies, with a particular focus on the CDC’s state and local policy recommendations and community-level strategies focusing on vulnerable populations [citations omitted from quotations, emphasis added by blog author].
- Universal use of face masks, including recommendations that communities “Issue policies or directives mandating universal use of face masks in indoor (non-household) settings” and “Plan for provision of face masks for specific populations if needed.”
- Physical distancing and limiting contacts. “At the community level, physical barriers and visual reminders might promote adherence to maintaining physical distance.”
- Avoiding nonessential indoor spaces and crowded outdoor settings, including “Issue policies or directives restricting some nonessential indoor spaces that pose the highest risk for transmission.” This includes “Indoor venues, where distancing is not maintained and consistent use of face masks is not possible (e.g., restaurant dining), [which] have been identified as particularly high-risk scenarios.” CDC also states, “Community-level policies can further reduce transmission by promoting flexible worksites (e.g., telework) and hours, as well as by applying limits to occupancy of indoor spaces and to the size of social gatherings.”
- Increased testing, diagnosis, and isolation. “Expanded screening testing should be implemented in a manner that promotes health equity for persons with limited resources or other barriers to accessing health care.”
- Prompt case investigation and contact tracing to identify, quarantine, and test close contacts. “Contact tracing is most feasible when the incidence of COVID-19 in the community or workplace is low or declining, when testing and reporting of results can occur quickly, and when most contacts can be reached and quarantined. When one or more of these conditions is not met or when local capacity is overwhelmed, health departments should narrow the scope of contact tracing activities and emphasize community mitigation measures. Investigations should prioritize persons who most recently received positive SARS-CoV-2 test results, as well as identify and quarantine household contacts and persons exposed in a congregate living facility, high-density workplace, or other setting (or event) with potential extensive transmission….Eliciting and reaching contacts in a timely manner is challenging, and quarantine can impose economic and financial burdens; adherence to quarantine might require provision of appropriate support services. Persons who receive positive SARS-COV-2 test results should also be encouraged to serve as their own contact tracers by informing close contacts that they have been exposed and encouraging those persons to quarantine, monitor for symptoms, and seek testing.”
- Safeguarding persons most at risk for severe illness or death. To protect such populations, “universal mitigation efforts are needed,” as is the “expan[sion of] access to testing, provision of support services, and messaging” within communities most at risk. In particular, the CDC points out that “COVID-19 has also disproportionately affected racial and ethnic minority groups. An age-standardized analysis of COVID-19–associated deaths reported to the National Vital Statistics System through November 25, 2020, found that Black persons accounted for 26.9% of COVID-19–related deaths, despite representing 12.7% of the U.S. population. Persons who belong to racial or ethnic minority groups are likewise disproportionately affected by the underlying medical conditions that increase risk for severe COVID-19 illness and death, likely because of long-standing inequities in social determinants of health. Members of racial or ethnic minority groups are more likely to experience lower socioeconomic status, to live in crowded housing, and possibly to be employed in occupations that require in-person work. In addition, access to health care might be limited, including obtaining testing and care for COVID-19.”
- Protecting essential workers (includes health care personnel, first responders, and grocery store workers, food manufacturing and agriculture, “especially among workers in meat and poultry processing facilities, with disproportionate effects among persons who belong to racial or ethnic minority groups”). “Protect essential workers through policies directing administrative and structural prevention as well as expanded testing.”
- Postponing travel and “Issue policies or directives mandating universal use of face masks on all modes of public transportation.”
- Increased room air ventilation, enhanced hand hygiene, and cleaning and disinfection.
- Widespread availability and coverage with effective vaccines, while also “Communicat[ing] that mitigation measures still need to be followed until community vaccination coverage is determined to be adequate.
Rapid Law & Policy Rundown
Given the length and scope of the above update, what follows below are links to other important recent reports, studies, articles, policies, and decisions.
- COVID-19 Vaccines:
- Vaccine distribution: We are getting closer to the approval of COVID-19 vaccines. This recent Health Affairs study puts proof behind the statement that “vaccines don’t stop infectious diseases, vaccination does.”
- Earlier this week, the CDC’s independent Advisory Committee on Immunization Practices recommended that health care personnel (broadly defined) and long-term care facility workers and residents be first in line to receive the COVID-19 vaccines expected to soon be approved for use.
- What about mandates? I, along with several other public health law and ethics experts, believe at this time we shouldn’t be focused on mandates, and should instead be “maximizing communication and minimizing barriers” to access. As I state in this USA Today piece, “What can we do to make this as easy as possible for people to say yes to? The best approach to be taking in the near term is engaging communities, answering questions, and letting people know what the benefits and risks are, where they’re going to be able to get access to it and that there are no costs associated with getting the vaccine.”
- This NY Times piece will give you an idea on where you might be in line to get access to a COVID-19 vaccine.
- While there is increased skepticism about COVID-19 vaccination, for ethical and legal reasons, the government should not pay people as an incentive to get vaccinated.
- Life Insurance. COVID-19 survivors worry companies will raise rates, deny coverage
- COVID-19 “Immunity Passports” would worsen economic inequality.
- The U.S. Supreme Court overturned a New York state policy that had restricted the size of religious gatherings in pandemic hot spots, raising significant questions about the ability to rely upon public health data to best control infectious disease outbreaks, and triggering more religion-based challenges to COVID-19 policies, such as a First Amendment challenge to school based closures in Kentucky that the Sixth Circuit recently overturned.